Dosing for PREVYMIS® (letermovir) in CMV R+ allogeneic hematopoietic stem cell transplantation (HSCT) patients
Download Dosing and Administration Card PDF
Once-daily dosing: start PREVYMIS as early as the day of transplant
- Start PREVYMIS as early as day 0 and no later than day 28 post-transplant.
- PREVYMIS can be initiated before or after engraftment.
- Following the completion of prophylaxis with PREVYMIS, monitoring for CMV reactivation in HSCT recipients is recommended.
Once-daily dosing
- Please see full Prescribing Information for proper preparation and administration of PREVYMIS IV infusion.
- PREVYMIS injection should be used only in patients unable to take oral therapy and patients should be switched to oral PREVYMIS as soon as they are able to take oral medications. If possible, intravenous administration should not exceed 4 weeks.
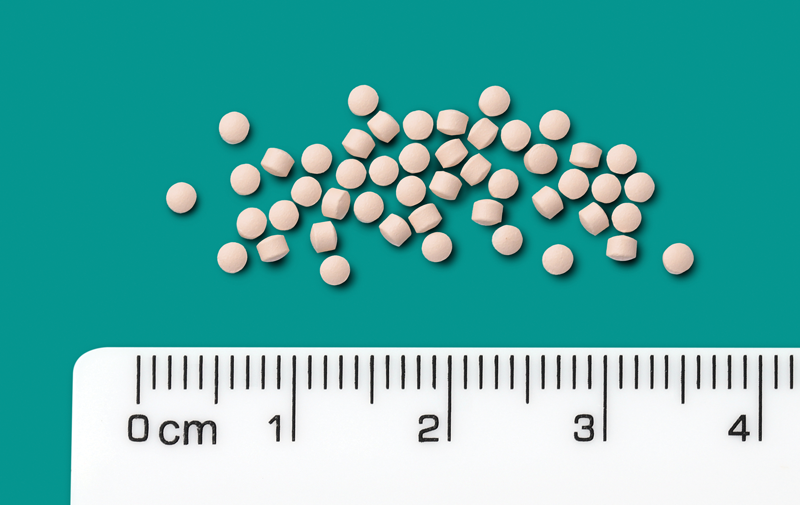
PREVYMIS is available in 3 dosage forms
Tablets
- Administer orally with or without food.
- Swallow tablets whole.
Oral Pellets
- Administer orally mixed with soft food or via nasogastric tube (NG tube) or gastric tube (G tube) mixed with water.
- Do not crush or chew.
- Instructions for Use should be followed for preparation and administration of PREVYMIS oral pellets.
Injection
- PREVYMIS injection must be diluted prior to administration.
- The diluted solution is stable for up to 24 hours at room temperature or up to 48 hours under refrigeration (this time includes storage of the diluted solution in the intravenous bag through the duration of infusion).
- Administer PREVYMIS through a sterile 0.2 micron or 0.22 micron PES in-line filter.
- Administer by IV infusion via a peripheral catheter or central venous line at a constant rate over 1 hour; do not administer as an IV bolus injection.
- PREVYMIS injection, which contains hydroxypropyl betadex, should be used only in patients unable to take oral therapy. Patients should be switched to oral PREVYMIS as soon as they are able to take oral medications. If possible, intravenous administration should not exceed 4 weeks.
- In patients with renal impairment, accumulation of hydroxypropyl betadex may occur. In adult patients with CLcr less than 50 mL/min and in pediatric patients with a similar degree of renal impairment (based on age appropriate assessment of renal function) receiving PREVYMIS injection, closely monitor serum creatinine levels.
- Animal studies have shown the potential for hydroxypropyl betadex to cause ototoxicity. The active ingredient, letermovir, is not known to be associated with ototoxicity.
- No dosage adjustment is necessary when switching formulations in adult and pediatric HSCT patients 12 years of age and older and weighing at least 30 kg.
- Dosage adjustment may be necessary for pediatric HSCT patients less than 12 years of age when switching between oral and intravenous formulations.
240 mg tablet
480 mg tablet
20 mg packet of pellets
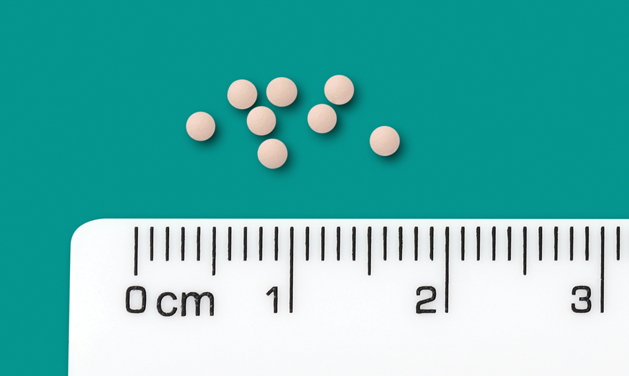
120 mg packet of pellets
240 mg/12 mL vial

480 mg/24 mL vial

Tablets, pellets, and vials not actual size.
Recommended dosage for HSCT patients 12 years of age and older
HSCT: Adult and Pediatric Patients 12 Years of Age and Older and Weighing at least 30 kg
- The recommended dosage of PREVYMIS is 480 mg administered orally or intravenously once daily.
- When PREVYMIS is administered orally, the recommended dosage is one 480 mg tablet once daily or two 240 mg tablets once daily.
- Four 120 mg packets of oral pellets once daily can be used for patients who cannot swallow tablets.
- For preparation and administration instructions refer to Preparation and Administration of Oral Pellets and Preparation and Administration of Intravenous (IV) Solution.
For pediatric patients less than 12 years of age or weighing less than 30 kg, refer to weight-based dosing in Table 1 (tablets or oral pellets) and Table 2 (injection) in the Prescribing Information.
Initiate PREVYMIS between Day 0 and Day 28 post-HSCT (before or after engraftment) and continue through Day 100 post-HSCT. In patients at risk for late CMV infection and disease, PREVYMIS may be continued through Day 200 post-HSCT.
Dosage of PREVYMIS should be adjusted when co-administered with cyclosporine.
Dosage Adjustment When CO-ADMINISTERED WITH CYCLOSPORINE for Adult and Pediatric Patients 12 Years of Age and Older Who Are HSCT Recipients
- If oral or intravenous PREVYMIS is co-administered with cyclosporine, the dosage of PREVYMIS should be decreased to 240 mg once daily in the following population:
- HSCT: adult and pediatric patients 12 years of age and older and weighing at least 30 kg
- If cyclosporine is initiated after starting PREVYMIS, the next dose of PREVYMIS should be decreased to 240 mg once daily.
- If cyclosporine is discontinued after starting PREVYMIS, the next dose of PREVYMIS should be increased to 480 mg once daily.
- If cyclosporine dosing is interrupted due to high cyclosporine levels, no dose adjustment of PREVYMIS is needed.
Following the completion of PREVYMIS prophylaxis, monitoring for CMV reactivation in HSCT recipients is recommended.
Recommended dosage for HSCT patients 6 months to less than 12 years of age or 12 years of age and older and weighing less than 30 kg
- The recommended dosages of PREVYMIS for pediatric HSCT recipients 6 months to less than 12 years of age are based on weight and shown in Table 1 (tablets or oral pellets) and Table 2 (injection) below and in the Prescribing Information.
- PREVYMIS can be administered orally (tablet or pellet) or intravenously once daily.
- Dosage adjustment may be necessary for pediatric patients less than 12 years of age when switching between oral and intravenous formulations (see Table 1 and Table 2 below and in the Prescribing Information).
Initiate PREVYMIS between Day 0 and Day 28 post-HSCT (before or after engraftment) and continue through Day 100 post-HSCT. In patients at risk for late CMV infection and disease, PREVYMIS may be continued through Day 200 post-HSCT.
Following the completion of PREVYMIS prophylaxis, monitoring for CMV reactivation in HSCT recipients is recommended.
Table 1: Recommended Daily Oral Dosage of PREVYMIS in Pediatric HSCT Recipients 6 Months to Less than 12 Years of Age or 12 Years of Age and Older and Weighing Less than 30 kg
*Refer to Preparation and Administration of Oral Pellets for dosing instructions.
Table 2: Recommended Daily IV Dosage of PREVYMIS in Pediatric HSCT Recipients 6 Months to Less than 12 Years of Age or 12 Years of Age and Older and Weighing Less than 30 kg
*Refer to Preparation and Administration of Intravenous (IV) Solution for dosing instructions.
Dosage Adjustment When CO-ADMINISTERED WITH CYCLOSPORINE for Pediatric Patients 6 Months to Less than 12 Years of Age or 12 Years of Age and Older and Weighing Less than 30 kg Who Are HSCT Recipients
If oral or intravenous PREVYMIS is co-administered with cyclosporine in pediatric HSCT recipients 6 months to less than 12 years of age, the dosage of PREVYMIS may require adjustment as shown in Table 3 below and in the Prescribing Information.
- If cyclosporine is initiated after starting PREVYMIS, the next dose of PREVYMIS should be the daily oral or intravenous dose co-administered with cyclosporine (Table 3 below and in the Prescribing Information).
- If cyclosporine is discontinued after starting PREVYMIS, the next dose of PREVYMIS should be the daily oral or intravenous dose administered without cyclosporine (Table 1 or Table 2 above and in the Prescribing Information).
- If cyclosporine dosing is interrupted due to high cyclosporine levels, no dose adjustment of PREVYMIS is needed.
Table 3: Recommended Dosage of PREVYMIS when Co-administered with Cyclosporine in Pediatric HSCT Recipients 6 Months to Less than 12 Years of Age or 12 Years of Age and Older and Weighing Less than 30 kg
*Refer to Preparation and Administration of Oral Pellets and Preparation and Administration of Intravenous (IV) Solution for dosing instructions.
For use in HSCT patients with renal and hepatic impairment
Use in Patients with Renal Impairment
- For adult patients with creatinine clearance (CLcr) greater than 10 mL/min and pediatric patients with a similar degree of renal impairment (based on age-appropriate assessment of renal function), no dosage adjustment of PREVYMIS is required based on renal impairment.
- There are insufficient data in adult patients with CLcr 10 mL/min or less or in patients on dialysis or in pediatric patients with a similar degree of renal impairment (based on age-appropriate assessment of renal function) to make PREVYMIS dosing recommendations.
- In adult patients with CLcr less than 50 mL/min and in pediatric patients with a similar degree of renal impairment (based on age-appropriate assessment of renal function) receiving PREVYMIS injection, accumulation of the intravenous vehicle, hydroxypropyl betadex, may occur. Closely monitor serum creatinine levels in these patients.
- Animal studies have shown the potential for hydroxypropyl betadex to cause ototoxicity. The active ingredient, letermovir, is not known to be associated with ototoxicity.
- The safety of PREVYMIS in adult patients with end-stage renal disease (CLcr less than 10 mL/min) or in pediatric patients with a similar degree of renal impairment (based on age-appropriate assessment of renal function), including patients on dialysis, is unknown.
Use in Patients with Hepatic Impairment
No dosage adjustment of PREVYMIS is required for patients with mild (Child-Pugh Class A) or moderate (Child-Pugh Class B) hepatic impairment. PREVYMIS is not recommended for patients with severe (Child-Pugh Class C) hepatic impairment.
Preparation and administration of oral pellets
PREVYMIS oral pellets can be administered:
- orally after mixing with soft food
or
- via NG tube or G tube mixed with water
Do not crush or chew.
Preparation and Administration Mixed with Soft Food
See Instructions for Use for details on the preparation and administration of PREVYMIS oral pellets mixed with soft food.
- Do not crush or chew PREVYMIS oral pellets.
- Mix PREVYMIS oral pellets with 1 to 3 teaspoons of soft food (such as applesauce, yogurt, or pudding) that is at or below room temperature. Do not use hot food.
- Administer entire mixture within 10 minutes of mixing PREVYMIS oral pellets with the soft food.
Preparation and Administration via NG Tube or G Tube
See Instructions for Use, Table 4 (NG Tube) and Table 5 (G Tube) below and in the Prescribing Information for details on the preparation and administration of PREVYMIS oral pellets via NG tube or G tube.
- Pour PREVYMIS oral pellets into a medicine cup containing room temperature water (see Initial Volume in Table 4 and Table 5 below and in the Prescribing Information). Do not mix PREVYMIS oral pellets with hot or cold (refrigerated) water.
- Wait 10 minutes. Do not shake or swirl the medicine cup. PREVYMIS oral pellets will not dissolve but will become loose or broken up. The entire mixture should be administered (see steps 3 and 4) within 2 hours.
- Stir the mixture with the syringe and administer entire mixture right away using the syringe and NG tube or G tube.
- Add room temperature water (see Rinse Volume in Table 4 and Table 5 below and in the Prescribing Information) to the medicine cup for rinsing, stir with a syringe and administer the entire rinse mixture using the syringe and NG tube or G tube.
- Flush the NG tube or G tube with the volume of water recommended by the NG or G tube manufacturer.
Table 4: Recommendations for Administration of PREVYMIS Oral Pellets Via NG Tube
Table 5: Recommendations for Administration of PREVYMIS Oral Pellets Via G Tube
Preparation and administration of intravenous (IV) solution
PREVYMIS injection is supplied in 30 mL single-dose vials containing either 240 mg/12 mL per vial (20 mg/mL) or 480 mg/24 mL per vial (20 mg/mL).
PREVYMIS vials are for single use only. Discard any unused portion.
Preparation Instructions
- PREVYMIS must be diluted prior to intravenous (IV) use. Only 0.9% Sodium Chloride and 5% Dextrose are chemically and physically compatible with PREVYMIS injection.
- Do not shake PREVYMIS vial.
- Inspect vial contents for discoloration and particulate matter prior to dilution. PREVYMIS injection is a clear colorless solution and may contain a few product-related small translucent or white particles.
- Do not use the vial if the solution is cloudy, discolored, or contains matter other than a few small translucent or white particles.
- Once diluted, the solution of PREVYMIS is clear, and ranges from colorless to yellow. Variations of color within this range do not affect the quality of the product.
- Do not use PREVYMIS injection with IV bags and infusion set materials containing the plasticizer diethylhexyl phthalate (DEHP). Use only with IV bags and infusion set materials that are DEHP-free. Materials that are phthalate-free are also DEHP-free. Materials that are phthalate-free are also DEHP-free.
- Use compatible IV bags and infusion set materials. PREVYMIS injection is compatible with the following IV bags and infusion set materials. PREVYMIS injection is not recommended with any IV bags or infusion set materials not listed below (note that PREVYMIS injection is not recommended for use with polyurethane-containing IV administration set tubing).
- IV Bags Materials:
Polyvinyl chloride (PVC), ethylene vinyl acetate (EVA) and polyolefin (polypropylene and polyethylene) - Infusion Sets Materials:
PVC, polyethylene (PE), polybutadiene (PBD), silicone rubber (SR), styrene–butadiene copolymer (SBC), styrene-butadiene-styrene copolymer (SBS), polystyrene (PS) - Plasticizers:
Tris (2-ethylhexyl) trimellitate (TOTM), benzyl butyl phthalate (BBP) - Catheters:
Radiopaque polyurethane
- IV Bags Materials:
- For the 480 mg or 240 mg dose, add PREVYMIS injection (see Table 6 below and in the Prescribing Information) into a 250 mL pre-filled IV bag containing either 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP and mix bag gently. Do not shake.
- For the 120 mg or 60 mg dose, add PREVYMIS injection into a pre-filled IV bag containing either 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP (see Table 6 below and in the Prescribing Information) and mix bag gently. Do not shake.
Table 6: Preparation of PREVYMIS Intravenous Solution for Doses of 60 mg or Greater
- For the 40 mg dose, prepare a dilution of PREVYMIS injection according to Table 7 below and in the Prescribing Information in either 0.9% Sodium Chloride Injection, USP or 5% Dextrose Injection, USP and mix bag gently. Transfer 20 mL from the prepared dilution into an appropriately sized IV bag or syringe. Do not shake.
Table 7: Preparation of PREVYMIS Intravenous Solution for Doses of 40 mg
Administration Instructions
- Administer the entire contents of the intravenous bag or syringe by intravenous infusion via a peripheral catheter or central venous line at a constant rate over 1 hour; do not administer as an IV bolus injection.
- The diluted solution must be administered through a sterile 0.2 micron or 0.22 micron polyethersulfone (PES) in-line filter. Do not administer through a filter other than a sterile 0.2 micron or 0.22 micron PES in-line filter.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration.
- Discard if the diluted solution is cloudy, discolored, or contains matter other than a few small translucent or white particles.
- The diluted solution is stable for up to 24 hours at room temperature or up to 48 hours under refrigeration (this time includes storage of the diluted solution in the intravenous bag through the duration of infusion).